Patients and Carers
This page is intended for patients and their carers who wish to learn more about blood cancers.
Blood Cancers: Understanding, Treatment, and Innovations – What You Need to Know
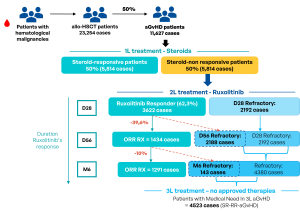
Graft-versus-Host Disease (GvHD)
Graft-versus-Host Disease (GvHD) is a serious complication that can occur after an allogeneic stem cell transplant, a common treatment for blood cancers such as leukemia, lymphoma, and myeloma. GvHD happens when the donated hematopoietic stem cells view the recipient’s body as foreign and start attacking healthy tissues and organs.
There are two main forms of GvHD: acute GvHD (aGvHD), that occurs within the first 100 days post-transplant, and chronic GvHD (cGvHD), that develops after 100 days or more. Both types can significantly impact survival rates and quality of life after stem cell transplantation. The symptoms of each form also vary significantly.

Expert Insights on aGvHD: Microbiota Disruption and Therapeutic Approaches – Prof. Florent Malard
Gut microbiome and Blood cancers: Improving Outcomes for Patients
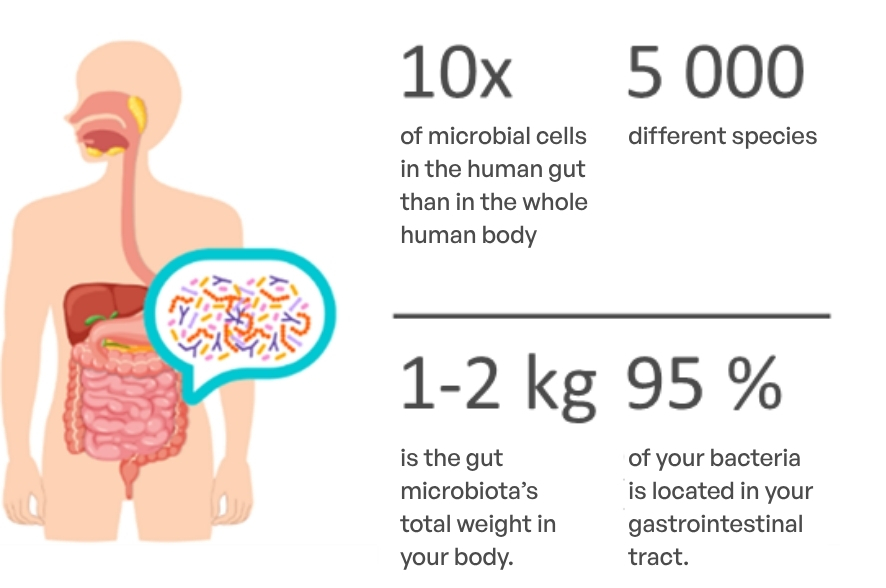
The gut microbiome—a complex community of billions of microorganisms living in our intestines—plays a crucial role in overall health. It is unique to each individual and affects not just digestion, but also immune function and the effectiveness of certain cancer treatments.
Click here for more information about gut microbiome.
Source : INSERM https://www.inserm.fr/dossier/microbiote-intestinal-flore-intestinale/